When it comes to treating opioid addiction, Suboxone treatment is the most commonly used method of medication-assisted treatment (MAT) in South Florida. Suboxone is a medication containing buprenorphine and naloxone that helps treat withdrawal symptoms and drug cravings in people who are trying to overcome opioid use disorder. There are many different types of medications used in medication-assisted treatment programs. However, Suboxone is one of the most popular options. It has been around longer than Vivitrol and Sublocade and is cost-effective.
Like other medications used in MAT, Suboxone is not intended to replace a comprehensive treatment program. It does not claim, nor is it proven to be the ultimate cure for opioid use disorder or opioid addiction. Instead, Suboxone is most effective when it is one component of an opioid treatment program. These treatment programs typically consist of detox, behavioral therapy, experiential therapies, and inpatient and outpatient rehab.
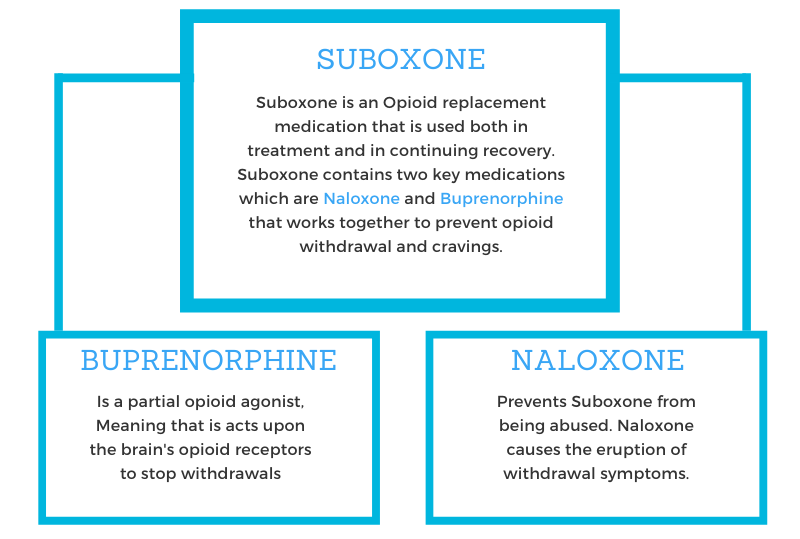
How do Buprenorphine and Naloxone Work?
Buprenorphine and naloxone are the two medications in Suboxone that help support recovery. The drug comes as either a sublingual strip or a pill, both of which are dissolved under the tongue. First, buprenorphine is a partial opioid agonist – meaning it attaches to the opioid receptors in the brain. As a result, other opioids cannot attach to these receptors. However, buprenorphine is an opioid itself, so individuals who take Suboxone during detox experience relief from their withdrawal symptoms. Some people are skeptical about buprenorphine because of this, but it is much weaker than other opioids of abuse.
Furthermore, naloxone, the other key medication in Suboxone, prevents misuse of the drug. It blocks the effects of opioids, so if a person uses an opioid while on Suboxone, he or she won’t feel the euphoric effects of the drug. In addition, if someone tries to abuse Suboxone, the naloxone in the drug may cause them to go into immediate withdrawals – something nobody wants to experience.
The Drug Addiction Treatment Act was passed in 2000, which extended buprenorphine prescribing abilities to community physicians rather than only specialized treatment providers. When naloxone was added to the mix in 2002, Suboxone quickly grew in popularity after proving itself as an effective method of assisting in the treatment of opioid use disorder.
How Effective is Suboxone?
Suboxone is used during many different stages of opioid rehab. Over time, it has proven to work as both a long and short term solution for individuals with opioid use disorder. When it is combined with an opioid rehab program, the drug helps eliminate cravings for opioids.
One study looked at Suboxone patients and regular opioid rehab patients for 12 weeks. The results demonstrated that participants who obtained counseling and Suboxone had substantially better outcomes than those who received the standard treatment regimen. Individuals who participated in medication-assisted treatment were less likely to use opioids and other drugs. Similarly, they were more likely to complete the duration of their treatment program. [2]
While the medication is extremely helpful in treating opioid use disorder, it is essential that it is used in tandem with a comprehensive opioid rehab program. After all, the relative success of Suboxone treatment is partly based on the length of time individuals remain in treatment.
What are the Benefits?
When people think of Suboxone, they often think of how it helps with cravings and opioid withdrawal symptoms. However, there are many other benefits to using this harm-reduction drug. Buprenorphine and naloxone are associated with the following.
- Better pregnancy outcomes in opioid-addicted mothers
- Lower relapse rates
- Reduced opioid overdose fatalities
- Reduced transmission rates of hepatitis C and HIV
- Higher retention rates in opioid rehab programs
- Over-all improved quality of life
- Relief for chronic pain
- Reduced stress levels
- Increased calmness and relaxation
Many people worry about the abuse potential of Suboxone. Fortunately, the unique combination of buprenorphine and naloxone reduces the abuse potential while still offering the same benefits of taking only buprenorphine. Suboxone is a schedule III drug, meaning it has less potential for abuse and addiction than drugs like methadone. Furthermore, since it is classified as a schedule III drug, any physician can prescribe Suboxone – increasing patient access to the drug.[1]
Who can Participate in Suboxone Treatment?
Suboxone should not be used by people who are unaware of the potential side effects and drug interactions. In addition, it should not be used as a way to avoid withdrawal symptoms in a person who doesn’t have a desire to get sober. Lastly, if a person begins taking Suboxone and experiences adverse side effects, he or she should stop treatment and avoid taking the medication.
The FDA explains that Suboxone is useful in treating opioid use disorder in adults over the age of 18. It is a great option for people in both inpatient and outpatient treatment settings.[3] However, before anyone starts Suboxone treatment, they should speak with their physician and/or an addiction specialist. Suboxone treatment isn’t right for everyone, so it’s important to adhere to professional advice.
Comprehensive Wellness Centers in Palm Beach, Florida offers Suboxone treatment as part of our opioid rehab program. Each of our medication-assisted treatment plans is highly individualized to meet the unique needs of each client. We understand that medication only isn’t a cure for opioid addiction, which is why our behavioral therapies and counseling techniques help individuals learn how to navigate daily life in sobriety.
Are you ready to get clean for once and for all? Don’t wait another day. Reach out to our addiction specialists in Palm Beach today.
References: